Hormonal Control of Calcium & Phosphate Metabolism & the Physiology of Bone
Introduction
Calcium is an essential intracellular-signaling molecule and also plays a variety of extracellular functions, thus the control of bodily calcium concentrations is vitally important. The components of the system that maintain calcium homeostasis include cell types that sense changes in extracellular calcium and release calcium-regulating hormones, and the targets of these hormones, including the kidneys, bones, and intestine, that respond with changes in calcium mobilization, excretion, or uptake. Three hormones are primarily concerned with the regulation of calcium metabolism.
Calcium & phosphorus metabolism
It is the free, ionized calcium in the body fluids that is a vital second messenger (see Chapter 2) and is necessary for blood coagulation, muscle contraction, and nerve function. A decrease in extracellular Ca2+ exerts a net excitatory effect on nerve and muscle cells in vivo (see Chapters 4 and 5). The result is hypocalcemic tetany, which is characterized by extensive spasms of skeletal muscle, involving especially the muscles of the extremities and the larynx. Laryngospasm can become so severe that the airway is obstructed and fatal asphyxia is produced. Ca2+ also plays an important role in blood clotting (see Chapter 32), but in vivo, fatal tetany would occur before compromising the clotting reaction.
Phosphorus
Phosphate is found in ATP, cyclic adenosine monophosphate (cAMP), 2,3-diphosphoglycerate, many proteins, and other vital compounds in the body. Phosphorylation and dephosphorylation of proteins are involved in the regulation of cell function (see Chapter 2). Therefore, it is not surprising that, like calcium, phosphate metabolism is closely regulated. Total body phosphorus is 500 to 800 g (16.1–25.8 mmol), 85–90% of which is in the skeleton. Total plasma phosphorus is about 12 mg/dL, with two-thirds of this total inorganic compounds and the remaining inorganic phosphorus (Pi ) mostly in PO4 3–, HPO4 2–, and H2PO4 –. The amount of phosphorus normally entering bone is about 3 mg (97 +mol)/kg/d, with an equal amount leaving via reabsorption.
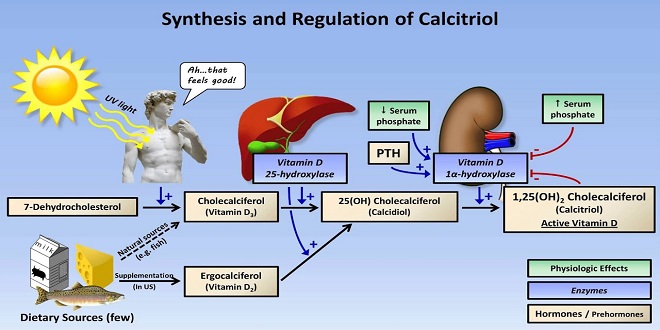
Mechanism of action
1,25 dihydroxycholecalciferol stimulates the expression of a number of gene products involved in calcium transport and handling via its receptor, which acts as a transcriptional regulator in its ligand-bound form. One group is the family of calbindin-D proteins. These are members of the troponin C superfamily of Ca2+-binding proteins that also includes calmodulin (see Chapter 2). Calbindin-Ds are found in human intestine, brain, and kidneys. In the intestinal epithelium and many other tissues, two calbindins are induced: calbindinD9K and calbindin-D28K, with molecular weights of 9,000 and 28,000, respectively. 1, 25-dihydroxycholecalciferol also increases the number of Ca2+–ATPase and TRPV6 molecules in the intestinal cells, thus, the overall capacity for absorption of dietary calcium is enhanced.
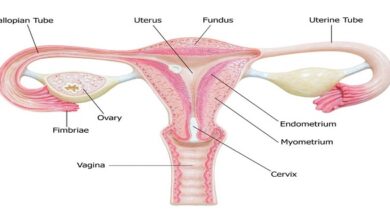
The parathyroid glands
Humans usually have four parathyroid glands: two embedded in the superior poles of the thyroid and two in its inferior poles. Each parathyroid gland is a richly vascularized disk, about 3 × 6 × 2 mm, containing two distinct types of cells. The abundant chief cells, which contain a prominent Golgi apparatus plus endoplasmic reticulum and secretory granules, synthesize and secrete parathyroid hormone (PTH). The less abundant and larger oxyphil cells contain oxyphil granules and large numbers of mitochondria in their cytoplasm. In humans, few are seen before puberty, and thereafter they increase in number with age.
Summary
Circulating levels of calcium and phosphate ions are controlled by cells that sense the levels of these electrolytes in the blood and release hormones, and effects of these hormones are evident in mobilization of the minerals from the bones, intestinal absorption, and/or renal wasting.
The majority of the calcium in the body is stored in the bones but it is the free, ionized calcium in the cells and extracellular fluids that fulfills physiological roles in cell signaling, nerve function, muscle contraction, and blood coagulation, among others.